“Hands Only” CPR or commonly referred to as “Compressions Only” CPR
I’ve been pondering this “gray area” for awhile now, it’s a common teaching point in our classes and it’s usually is followed with many questions from our students. “Hands Only” CPR or commonly referred to as “Compressions Only” CPR is just that, the utilization non-stop compressions during CPR that does NOT involve Ventilations via Mouth-to-Mouth or Face Shield. This was introduced back in 2008 by the American Heart Association as a way to get bystanders to perform Compressions (notice I didn’t say CPR) in the event of a witnessed Cardiac Arrest. Does it work? Sure it does. Is it as successful as proper CPR that utilizes a Compression:Ventilation ratio along with the use of an AED? Not exactly. But is it better than doing nothing? Absolutely. This is the “gray area” I was talking about, in this post I’ll do my best to explain the differences between proper CPR and Hands-Only CPR, some things to consider, and what I personally think about both practices.
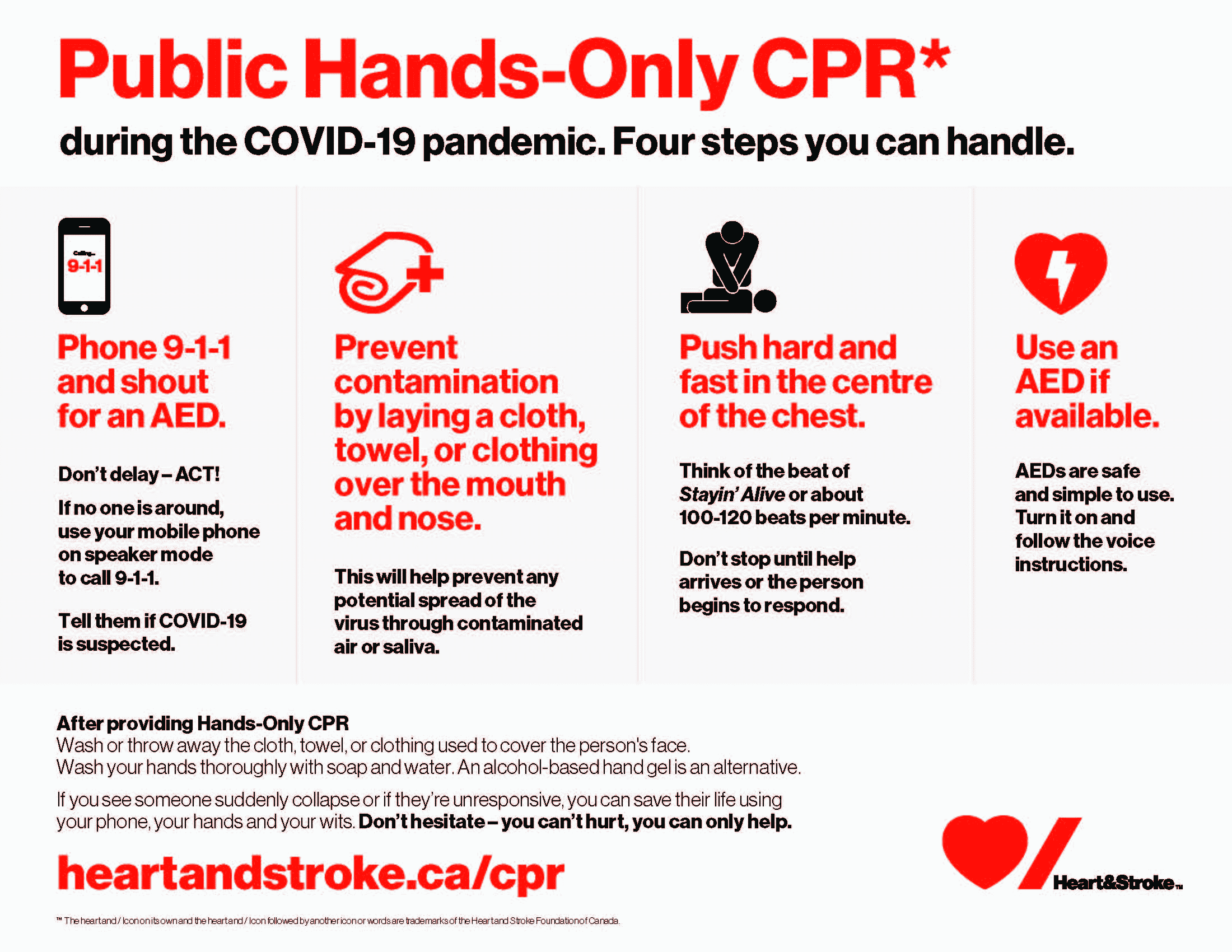
(THIS PSA BELOW BECAME VERY POPULAR DURING THE COVID-19 PANDEMIC)
Please note this is my Personal opinion on the subject which does NOT reflect any organization including the American Heart Association, the American Red Cross, the American Safety & Health Institute, or even IGH Health, Fire, & Safety because in my mind, this is truly a personal judgement call that will be assessed and acted upon during an actual Cardiac Arrest event. Every situation, patient, and rescuer is different so I believe we must stay fluid in our decision making process.
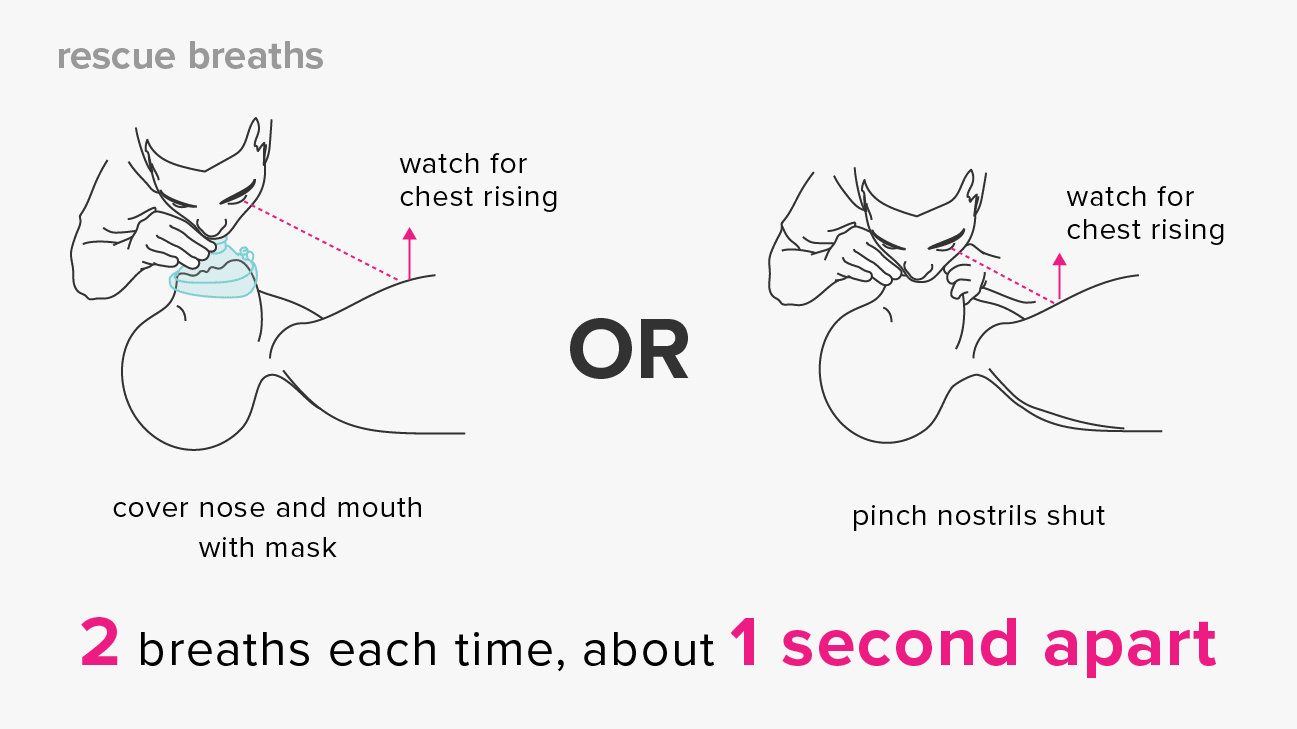
Normal, or proper, CPR (Cardiopulmonary Resuscitation) in the Public setting involves the use Compressions, Ventilations, and the AED. Compression’s take over the process of circulating blood and oxygen throughout the body to perfuse the vital organs since the heart is no longer “pumping” adequately. Ventilations provide Oxygen to the lungs which travel through the alveoli (tiny air sacs in your lungs) and it is then transferred to the circulatory system, throughout your body, and to your vital organs; NOTE that Ventilations cannot be performed without Compressions, the Circulatory system must be moving or “circulating” to pick up Oxygen from your lungs (alveoli) to transport it. The AED then provides Defibrillation if your patient is in V-Tach or V-Fib, which are the only two shockable heart rhythms. You can read more about AED’s on our other blog post “The Almighty AED” if you’d like, but today we’re just going to focus on Compressions and Ventilations. So Compressions and Ventilations go hand-in-hand, on a typical Adult Patient we teach a Compression:Ventilation Ratio of 30 Compressions to 2 Ventilations. The compressions get your Circulatory System moving again, and the Ventilations supply your Circulatory System with Oxygen. Think about it like this, if your Circulatory System is the Highway, than the Oxygen “particles” are like cars, if the Highway is shut down there are no cars moving, that’s why you’ve never heard of “ventilation only CPR”.
Now, “Hands-Only CPR” only involves the use of Continual Compressions, which means the rescuer will be performing non-stop compressions at a rate of 100-120 Compressions per minute, no ventilations needed. The only time a rescuer should stop during Hands-Only CPR is if they have an AED and it’s either Analyzing or Shocking, just remember you can absolutely still use an AED with Hands-Only CPR. These continual compressions provide a great source of circulation for the body since they’re non-stop and it still provides a good chance of patient survival.
So why do traditional CPR over Hands-Only CPR or vice-versa? I believe it comes down to a few deciding factors, there are many more than these three but we’ll start here:
- Quality of Compressions/Ventilations
- Patients Size/Age
- Bodily Fluids
Quality of Compressions/Ventilations: In a hospital or EMS Setting we’re trained to perform continual compressions and continual ventilations once an advanced airway is established, such as an ET Tube, because we no longer need to confirm chest-rise as our main source of proper feedback unlike Public or BLS CPR. In Public CPR or Basic Life Support we must stop Compressions to visualize chest rise during Ventilations, if there is no chest rise, there is no adequate transfer of oxygen. One of the biggest issues we see during CPR are poor ventilations, if you or another rescuer are providing subpar ventilations you might as well not do them because now you’re taking time off of compressions with no benefit. Our goal with compressions are to build up a “mechanical blood pressure”, and if we’re doing them properly we may build up a blood pressure close to 80/30. (Normal BP is 120/80) So it’s not perfect but it works right? The problem is that it may take us 30-60 compressions to build up to that 80/30 BP, which can take work and time, then for every SECOND you’re not doing those compressions their BP can drop 10 points! So if you have a good team of rescuers around you, a 30:2 ratio would work just fine, but if you’re struggling with compressions and ventilations you may just be doing more harm than good by increasing time off of the chest. Please remember, COMPRESSIONS ARE KING and to always reduce the time off of the chest.
Patients Age: Another thing to consider is the patients size and age. Adults are fully grown and developed, this means that even after a Cardiac Arrest they still have a decent amount of Oxygen left in the Circulatory System that can be transported and to perfused the vital organs. Children on the other hand are not fully developed nor are their organs and they do not have a circulatory system large enough to contain a decent supply of oxygen. In simple terms, Ventilations are more of a priority for Infants and Children than fully grown Adults.
Bodily Fluids: It’s no secret that you may come into contact with blood, sputum, and vomit during a cardiac arrest. There is a decent amount of physical damage being performed during CPR and when you’re ventilating via Mouth-to-Mouth or Rescue Mask/Barrier (no Advanced Airway) you’re pushing air into the lungs AND stomach, when the stomach becomes pressurized everything (vomit/blood/sputum) comes up and out, this one of the biggest problems with bystander CPR, the inability to create a true barrier between patient/rescuer to minimize the chances of transmittable diseases.
So those are a few things that run through my mind and I would take into consideration before performing Hands-Only CPR or Traditional CPR. So when students ask me what I would do in a situation where I don’t have a mouth barrier or AED it goes a little like this… (Remember, this is a personal opinion).
Any Infant or Child that goes into Cardiac Arrest I will absolutely do Mouth-to-Mouth and Traditional CPR, this also goes for any Adult that is my family member or close friend, most likely you’ll know of any transmittable diseases they may or may not have. The only time I wouldn’t perform Mouth-to-Mouth is if I witness an Adult I don’t know, or I’m not familiar with, go into Cardiac Arrest. I would then perform continual compressions. That being said, anytime I do have a Ventilation Barrier available I would perform compressions AND ventilations no matter age, size, bodily fluids, etc. (Which I always carry with me).
I hope this post explained the differences between Traditional/Proper CPR vs. Hands-Only/Compressions-Only CPR along with some considerations to take in mind if you’re going to perform Mouth-to-Mouth. At the end of the day, they’re both great options and doing SOMETHING is better than doing NOTHING. Also, one last thing to consider, you will never have to make that tough decision if you’re prepared and you buy a Rescue Mask, these things are great and provide wonderful ventilations while keeping a rigid barrier between you and your patient. They’re around $7 on Amazon and may be the difference between life and death for somebody one day, seems like a pretty “no-brainer” investment to me! Here’s a picture and a link to a Google Search if you’d like to learn more about these.

Thanks for reading, and as always, if you ever have any questions or comments please feel free to reach out to our office!
Brent Bousquet, President
IGH Health, Fire, & Safety
Office: (817) 809-8677
Website: www.ighsafety.com
